Monday Ellie had an appointment at the Synagis clinic (where
she gets a shot to prevent RSV). This
was her first time getting this, but she did fabulous. Later on Monday we had a family chiropractic
appointment and we all left feeling much better than when we arrived. Ellie seems to prefer looking to the left
when she’s laying down… so we’re trying to see what Dr. Josh can do to help her
here. Andrea, the physical therapist,
said that if she continues to show preference to one side, Ellie may need to
wear a “cap”. Noooooo… not the
helmet! We’re trying to be diligent at
turning her head right when she’s laying, but that little booger makes up her
own mind most times.
Tuesday was an awful day at home. I logged on to my work computer at 5am and
everything went into turtle mode. When I
did a restart on it, my computer did all kinds of techy mumbo jumbo and then
froze on the “starting windows” screen.
I called our help desk and the IT guys said, “yeah, your hard drive is
in the process of crashing”.
Excellent! So I was stressing because
I had several things that I needed to get out the door… like, yesterday… and
now had no way of doing them. Totally my
fault for procrastinating… but some of the reports were in progress… and now
needed to be handed off to get them to clients on time. I know – this means nothing to you… haha… but
it was NOT a fun way to start my day and I felt awful for handing tasks over to
my coworkers (who were willing to take on last-minute tasks ever so
graciously).
Tuesday afternoon, we saw Deb, our Home Health nurse. The boys are crazy about her. They always greet her at the door and talk
her ears off the whole time she’s at oour house. She usually lets them wear her stethoscope and
listen to their own heartbeats and tummies with it. No wonder they love her so much.
I was only supposed to work a half day Wednesday morning,
but couldn’t do much more than field emails from my phone while I waited for my
new laptop to arrive. It was delivered
just before I had to jet out the door to head to Dayton. We had 3 appointments at Children’s that day
and I was sweating the audiology appointment pretty seriously.
First stop: GI. This
was the first time we got a chance to meet our gastroenterologist. He was great, but he said he wasn’t happy at
all. This made me nervous, but he was
mostly just concerned that we were making things much harder than they had to
be. First, he wanted to get us set up
with a continuous feed pump to use at night and while I was working. Bonus!
He was also concerned that we didn’t have a plan to do much with the NG
tube yet. I didn’t know that NG tubes
should only be in for a few weeks. He
said that after 6 weeks, you can run the risk of doing permanent damage to the
nose/nasal cavity because of the tube.
You can also start seeing permanent damage to the esophagus (because the
sphincter at the top of the stomach is always open to accommodate the tube and
can let stomach acid bubble up into the esophagus). Since Ellie has already had her NG tube for 4
weeks, he wanted to get her scheduled to put in a G tube (or G button) as soon
as possible. He said we’d have to check
with cardiology before we could make any real surgery plans, but this was the
route he’d suggested. He also prescribed
Prilosec for Ellie after I told him about her daily crying episodes. They were no longer at night (praise God),
but they were still during the day. He
said we could try that and see if maybe the crying is related to reflux… which
could be the case, even though it didn’t happen after every feeding.
Second appointment: Audiology. Ellie was sleeping when we arrived in
audiology – which was great because she HAD to be sleeping for the test. Of course, once we were back in the testing
room, she wanted nothing to do with sleep.
Nichole, the sweet lady who was running the test, just kept saying, “I’ll
let you try to get her to sleep and I’ll be back in a few minutes”. She did this 4 or 5 times in the hour we were
down there… to no avail. Ellie refused
to sleep. Nichole set us up for another
appointment next week, but on the way out let me know that she’d be in the
office until 5pm, so if I was able to get Ellie to sleep at some point, I could
try bringing her back to do the test. By
the time I got out of the elevator on my way up to cardiology, Ellie was sound
asleep. Little turkey.
On the scales in cardiology, Ellie weighed 3.855 kg (or 8
pounds, 8 ounces). Dr. Luby was thrilled
with her weight gain and was amazed at how relaxed Ellie looked in her
breathing. I was excited to tell her how
alert Ellie had been lately and that she was now rolling over and showing
off. I also told her how Ellie didn’t
want to cooperate in audiology. We had
to laugh. We talked about our GI
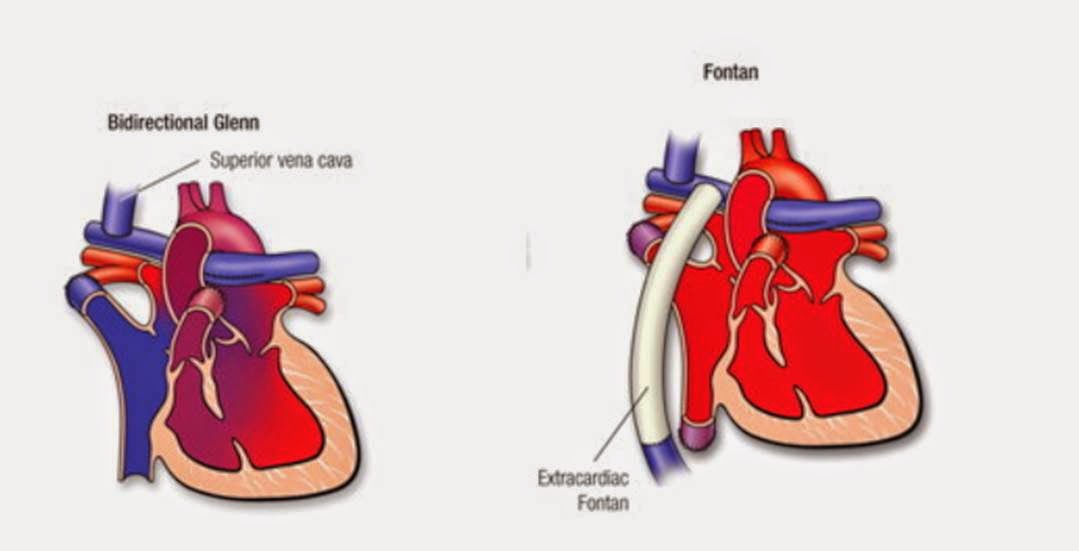
appointment and discussed the pros/cons of the NG tube vs. the G tube. Dr. Luby agreed that we didn’t want to risk
permanent damage to the nose and esophagus with the NG tube and she thought a G
tube would be a good idea… but not before heart surgery. She explained that the placement of the G
button (on a torso as small as Ellie’s) would be just a centimeter or two away
from where her incision would be for open heart surgery. The risk of infection trumps the risk of
damage from the NG tube. However,
because Ellie was looking so healthy and doing so well a t this point, Dr. Luby
thought it was a good idea to bump up surgery so that we didn’t keep the NG
tube in for a ridiculous amount of time.
She suggested surgery in a month.
(gulp… a month?) That’s scary…
but it’s scary no matter when it happens and if I’ve learned anything along
this journey, it’s that this woman knows what she’s talking about! If Dr. Luby says that Ellie is strong enough
and will do well in surgery, then Ellie is strong enough and will do well in
surgery. Dr. Luby was contacting the
surgery team at Cincinnati Children’s and told me that they’d be in touch with
us soon. I don’t know how soon is “soon”,
but we haven’t heard from them yet. It
looks like she’ll be having surgery before the end of the year, though, as long
as the surgeon concurs with what Dr. Luby suggests. Dr. Luby would also contact GI and let them
know that we’re holding off on the G tube placement. She said, “they may think I’m a Prima donna,
but I’m okay with that. They always have
to fold to what the cardiologist says in this kind of a situation”. Excellent!
If she needs a G tube after surgery, that’s not a problem at all.
Now… as for this hearing situation that I’d been sweating
for a few weeks: I was able to get Ellie
to sleep again as we left cardiology and I asked the nurse to call down to
audiology and see if Nichole would take us back. It worked out and we headed straight
down. Ellie woke up as the ear muff
things and electrodes were placed on her head, but went back to sleep shortly
thereafter. Nichole was able to run the
test and hallelujah, Ellie passed on both ears.
My heart was jumping for joy.
Nichole said that they couldn’t really test behavioral responses until
Ellie was 8 or 9 months old (and the issues I saw were behavioral), but she
said, “Ellie has the ability to hear… there is nothing indicating that she
cannot hear”. YAY!! My concern in this whole matter wasn’t with
how this could impact our family. I’d
have no problem learning sign language and interpreting for her the rest of my
life if that was what I needed to do. I
know our family would learn with us and it would have been just fine
there. My concern was for our little bug
when she entered school. There are few
things that make you an island quite like a language barrier… and I didn’t want
Ellie to have to deal with that on top of anything else that she might already
find as a barrier. Can you tell that I
prepare myself for the worst when I go in for testing and such? That may sound awful, but I figure that if I
mentally prepare for the worst, then anything less than the worst case scenario
is means for celebration, right? So we’ll
see later if her behavioral responses to sound are different than what we’d
expect… or maybe we’ll just find out that she’s incredibly laid back and doesn’t
really startle. Bonus! For now I’ll celebrate the fact that she IS
able to hear. Good stuff.
After a very long day bouncing all over the hospital, it was
finally time to head towards home and pick up my boys. We had dinner with good friends and I tried
to catch up on some work when I got home.
I was ready for a calmer day on Thursday. Around 8:30pm, the medical supply company had
a delivery truck driver at our door to deliver the feed pump and equipment to
us. As I unpacked it, I saw that we had
an IV stand that went with it that could be wheeled around the house. Brandon said, “aww, man… I was hoping to keep
IV bags out of our house until we were like 90.” So, we’re feeling extra old with all of the
random medical stuff around our house, but I have to say that the pump is
pretty amazing! I know it makes me sound
totally lazy, but now I only have to wake up at night if Ellie needs her diaper
changed. Score! This momma can sleep… and sleep is priceless.
Thursday morning, just before going into a meeting with my
supervisor, Ellie wiggled one little finger out of her mitten and managed to
pull her feeding tube out again. What a
turkey! So, in my meeting, I told my
supervisor that I’d need to leave work a little early to make it back down to
GI in time for an open appointment.
Silly Ellie! She either likes the
attention she gets at Children’s or she likes the car rides to Dayton. The boys went with me on this trip and Lance
said, “Where are we going, Mommy?” “To
GI”, I said. So the whole time he was
asking where we were going and then repeating everything I said. It was adorable listening to him try to say “Orthopedics”
(the closest x-ray area to GI). And I’m
endlessly amazed at how accommodating the staff members are of the boys. I love that they make it an adventure for
them to come along. The guy who did the
x-ray [each time they place a new tube, they have to do an x-ray to make sure
it’s in her stomach] brought the boys into the office with him while I held
Ellie for the x-ray and let them pick out stickers. The front desk greeters gave the boys a
puppet show and more stickers. And of
course, there are those little bus wagons that they get to ride in. Adventures all around! We stayed with the Skinner kids for a while
that afternoon, then the boys were off to Tracy & Josh’s house for the
night to hang out with their “friends” (cousins), who were all off school on
Friday.

I'm a rotten turkey who rips her tube out - in her jammies and sleep sack here :)
[sorry this is so out of focus]
Kaleb loves to ride the rocking horse in the waiting room for the GI clinic
On Friday morning, Ellie had her 2 month well child visit
with Dr. Taylor. She weighed 9 pounds
even on that scale (she always weighs quite a bit more at this office than at
the cardiologist). Big girl! This puts her at the 66th
percentile on the chart for girls with Down syndrome (and the 3rd
percentile for typical girls). So, she’s
still very much a peanut… but she’s growing beautifully. I mean, for every kid that’s always above the
90th percentile (Kaleb), there’s another out there that has to
occupy the lighter end of the spectrum, right?
After work, I went to pick up those rotten boys of ours from Tracy’s. A quick dinner at home and we were off again –
me to visit with a good friend Cindy and the kiddos with Daddy to go to Grandma
and Grandpa Maier’s house. The boys
would be spending the night with Grandma and Grandpa so that I could spend my
Saturday morning at Girls of Grace at church with family and friends.

Holy rainbow colors, batman! I love it. Our pretty girl in ruffles on Friday.
After Brandon got off work on Saturday, we went up to
Cridersville to scoop up the boys, then to Lima to meet with the Beech family
for dinner, then to Chuck E. Cheese’s for the kiddos. The kids were beyond tuckered out by the time
we made it to church this morning and took amazing naps for us this
afternoon. Ellie bug was super grumpy
today – just letting us know that she rules the household, I guess. Looking forward to next week where we only
have Home Health and therapy appointments (four appointments are much more
manageable than 9 in a week)! I think I’m
going to go to bed early tonight (can I tell you how awesome that continuous
feed pump is again??). G’night friends –
thank you, again, for following along.
All the prayers you lifted for Ellie’s hearing were surely answered this
week!
Snuggling with Mommy and giving ornery smiles. I finally caught one...
she's sticking her tongue out w/ it... but I'll take it.