Shortly thereafter, the cardiac team made rounds and they talked
to us about the fits and a plan moving forward.
Since it looked like the EEG was ruling out seizures, the next likely
explanation is that these are autonomic storms (exactly what we’d talked with
neuro about). They would need to do an
MRI to confirm this. However, for Ellie
to have an MRI, she’d have to be sedated again… and with her reaction last
time, they’d need to have the cardiac anesthesia team present for this. They also let us know that she’d possibly
need to hang out the in Cardiac ICU after the MRI, so they weren’t rushing this…
they wanted to make sure they could schedule the right anesthesia team and
such.
Almost as soon as the cardiac team left our room, Dr.
Morales (our surgeon) came in to do the surgery consult that we were supposed
to do next week. We were so excited to
get to meet him… but that excitement turned to a feeling of total defeat in a
matter of minutes. He said that Ellie’s
echo showed that her AV Canal defect was unbalanced. Unbalanced to the point where her right
ventricle looked inadequate to function (even after surgery). He gave us a quick anatomy lesson and
reminded us that the non-oxygenated blood from the body dumps into the right
atrium from the superior vena cava (SVC), which brings blood from the head and
upper body, and the inferior vena cava (IVC), which brings the blood up from everything
below the heart. In Ellie’s heart, the
volume that is dumped into the right atrium will not fit into her tiny right
ventricle (where the blood is held and then pumped to the lungs to pick up
oxygen). So, the solution is a different
surgery than we were originally thinking.
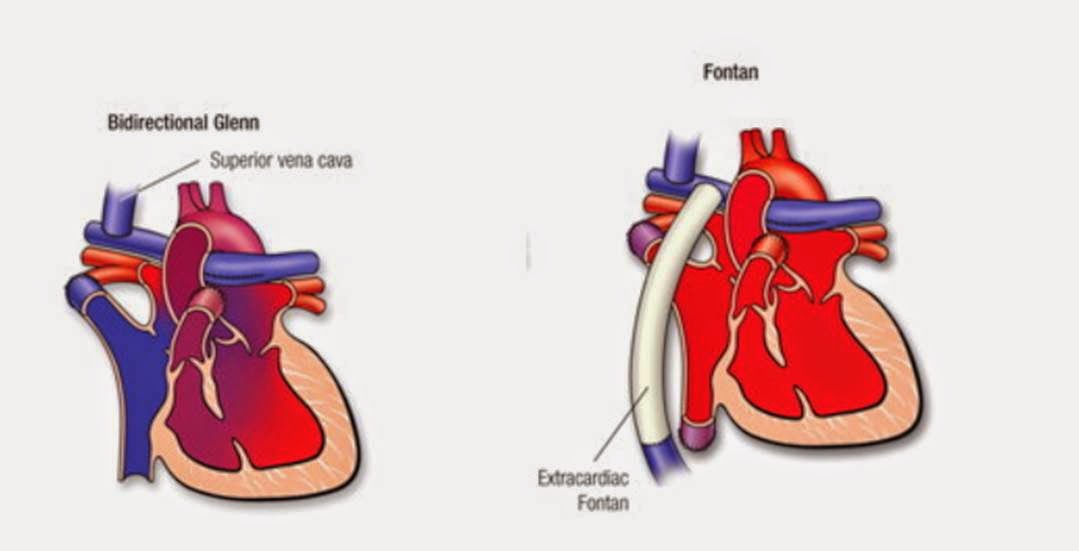
He’d have to do what is called a Glenn Operation first, where he will
disconnect the SVCs (Ellie actually has 2 of these instead of one… overachiever)
and connect them directly to the pulmonary arteries (arteries that carry blood
from the right ventricle to the lungs).
If Ellie does well with this, and her right ventricle can still handle
the volume of blood from the IVC, then she’d be good for a few years before
additional surgery would be needed. If
Ellie’s right ventricle cannot handle the volume of blood from the lower part
of her body, then an additional procedure would be needed (called a Fontan Operation). This procedure would direct the blood from
the IVC to the pulmonary arteries, as well.
Essentially, Ellie’s right ventricle is useless. These surgeries would make it so that Ellie’s
heart will work as just one pump instead of two. Her heart will only pump blood to her body,
like it’s just using the left side of her heart. Is this scary? Terrifying!
The scariest part about this for me is that if the operations are not
successful, the only other option is a heart transplant. So… these operations HAVE TO WORK. Below is a diagram of each procedure, if that
helps you understand my mumbo jumbo here.
Before we can think about surgery, we have to get to the
bottom of these episodes, or storms. A
storm would have catastrophic consequences on her post-surgery body. I don’t know why we didn’t think about this
before… but it was suddenly so obvious when he brought it up. A newly mended heart simply couldn’t handle
the stress that’s put on her heart and lungs during these episodes. That is our top priority right now… to figure
these out and treat them. Priority
number two is to make sure Ellie isn’t under respiratory distress and doesn’t
have any airway obstruction. We know she
has this now, we know that it’s very common in kiddos with Down syndrome. We also know that it makes the heart
procedures we’re now looking at much riskier.
If there is too much pressure in her pulmonary arteries, the blood will
not be able to passively flow into them (remember, blood will no longer “pump”
into the lungs). Ugh!
For now, they’re putting Ellie on a beta blocker called
propranolol as a maintenance medication to prevent the autonomic storms, at
least until we can get her in for an MRI sometime next week. Dr. Morales told us to expect to be here for
at least another week – maybe two so that we can get to the bottom of a few
things. They’re also going to do a heart
catheter sometime early next week to get a better idea of what her pulmonary
hypertension looks like. Sooo… it’s time
to get comfy. We went home quickly today
to pack up additional supplies and to visit with the boys for a while. Then we headed back to Cincinnati to set up
camp. It’s not bad here, it’s about the size
of a college dorm room. Except this
time, our roommate is a beautiful 10-pound ball of stress and the tests DO
actually have an impact on real life. This
is the hardest day we’ve had, in my opinion… and so far I’ve melted into B and
my dad and let the stress of it all run down my cheeks and onto their
shirts. Tomorrow is a better day, I know
that. In a weird way, I am so incredibly
thankful that she did not do well with sedation on Wednesday. If she had, we would have been sent home and
we would be dealing with respiratory distress at home. Also, these fits she’s been having (which
everyone kept saying was just colic wouldn’t have been addressed. Like I said earlier, not addressing these
would be catastrophic post-op). So, pray
for our baby, please… this is a harder road than we originally thought we’d be
traveling… and the first road wasn’t all that much fun. We’re hanging in there, though… we know that
God’s got this and He has a plan for our little bug.
Thank you for your prayers and for following along with our
story.
I'm praying for Ellie and your family. As hard as it is to b so far away, you are in the best of the best hospitals. Be strong and courageous, do not be discouraged do not be afraid for the Lord God will be with you wherever you go. Joshua 1:9
ReplyDelete